Esophageal Varices
- Cirrhosis of liver: In this condition, a healthy liver tissue is replaced by a scar tissue, which in turn blocks the circulation through the liver. Various diseases can cause cirrhosis such as viral infection of a liver, alcoholic liver disease, fatty liver, cystic fibrosis and biliary atresia. Cirrhosis accounts for 40 percent probability for esophageal varices.
- Thrombus formation: Formation of thrombus (clot) in the portal vein can cause esophageal varices.
- A parasitic infection: Infections such as Schistosomiasis can obstruct the portal vein leading to increase in pressure.
- Budd-Chiari syndrome: Interference with outflow of blood from liver due to formation of clot.
- Vomiting blood or black tarry blood or blood in stool;
- Lightheaded, dizzy;
- Loss of consciousness;
- Yellow eyes;
- Swollen abdomen;
- Pain abdomen.
- Esophagogastroduodenoscopy (EGD) to evaluate whether there is any evidence of bleeding, and help stop bleeding.
- Ultrasound of liver, CT and MRI scans to check liver structure and blood flow.
- Blood tests to check liver function and cause of liver disease.
- As there is increased pressure in the portal veins so beta-blockers such as propanolol should be given to minimize the pressure.
- The dilated veins need to be compressed, therefore a medication is injected into the swollen veins.
- In order to prevent bleeding from the varices, the dilated veins are tightly tied off with the help of endoscope.
- As there is increased chance of bleeding from varices, patient should be closely monitored for the sign and symptoms of hemorrhagic shock such as cold clammy skin, tachycardia, a drop in blood pressure, decreased urine output, restlessness, and weak peripheral pulses.
- If bleeding occurs and is present in vomit and stool, our major concern should be to stop bleeding as quick as possible.
- Intravenous fluids should be started to restore the lost fluid volume and correct the electrolyte imbalance.
- Blood Transfusion may be required.
- In order to reduce the pressure in the swollen veins, a drug called octreotide is administered which works by reducing the blood flow.
- Bleeding can be stopped from the varices by reducing the pressure in the portal vein which can be done by placing a stent in the liver through a catheter. The stent connects hepatic vein with the portal vein which provides extra pathway to carry blood to the heart. This procedure is called Transjugular Intrahepatic Portosystemic Shunt (TIPS).
- If all other options fail or are not viable, the patient should be considered for a liver transplant.
- Shock features like cold and clammy skin, perspiration, fast and feeble heart rate, decreased urine output, restlessness.
- Feeling dizzy, light headed.
- If blood is present in your vomitus or stool, you should always go for a treatment urgently.
- If your skin and eyes become yellow.
- If you have distended abdomen with or without pain, and swollen legs.
- Change in mental status or confusion.
- Avoid drinking excess alcohol.
- If you already have liver disease, stop alcohol completely.
- Do not use illegal intravenous drugs.
- Get checked if you have yellow eyes.
- If you have cirrhosis of liver, get Endoscopy to check for varices.
- Get vaccinated against Hepatitis B and if necessary against A.
- Avoid unnecessary medication.
- Regular blood tests to check liver function if you are taking medicine that can harm liver.
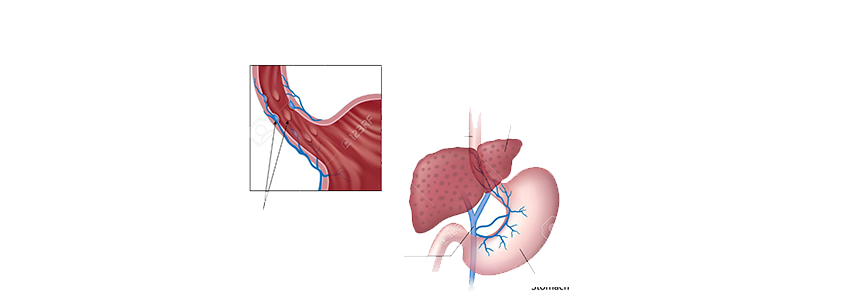
Esophageal varices are abnormally swollen veins in the lining of the lower esophagus. Most of the time, esophageal varices develop due to obstruction in the portal venous circulation (blood flow through the liver) but mainly it occurs when a healthy liver tissue is replaced by a scar tissue.
Due to the obstruction in portal vein, venous blood from abdominal organs and peripheral circulation cannot pass through the liver. As a result, a bypass circulation is created through other small blood vessels nearby. But due to the decreased capacity to handle the increased blood flow, gradually the small veins enlarge and swell. Eventually bleeding occurs due to decreased elasticity and increased pressure in the small parallel veins.
Causes
Some of the causes for esophageal varices are listed below:
Symptoms
Esophageal varices may remain silent or present with bleeding. Person may have symptoms due to the underlying cause that is responsible for the varices. Common symptoms include:
Treatment options
Treatment for esophageal varices depends upon the underlying cause and symptoms for which the following investigations may be done:
The main goal of treatment is to prevent esophageal varices from rupturing and bleeding. Bleeding mainly can be prevented by minimizing the pressure in the portal veins. Following treatment options should be followed in case of esophageal varices:
When to seek a medical help
Bleeding from esophageal varices is an emergency condition and can be fatal if not managed on time. Patients can lose massive amounts of blood in a short time. One should visit a doctor if following features may present:
Prevention
Esophageal varices is prevented by preventing a liver disease. You can follow these guidelines to help prevent this condition:



Send us your feedback on this article