Protein Energy Malnutrition
- Poverty: lack of access to high quality protein rich diet.
- Low birth weight: Malnourished mothers have a high incidence of low birth weight and growth retarded babies with poor nutritional reserve leading to PEM.
- Infections: Diarrhea, pneumonia, malaria, measles, whooping cough and tuberculosis precipitate acute malnutrition. Malnutrition impairs immunity which, in turn, makes individuals more susceptible to infections.
- Feeding habits: Lack of exclusive breastfeeding for first 6 months makes the child prone to early onset of malnutrition. On the other hand, prolonged breastfeeding and late introduction of supplementary foods may also increase the risk of undernutrition.
- Social factors: Repeated pregnancies, inadequate child spacing, food taboos, broken homes and separation of child from parents are important social factors that may also play a role in the etiology of PEM.
- Malabsorption: A number of malabsorption conditions can increase the risk of PEM in adults and children. These include cystic fibrosis, coeliac disease, etc.
- Traditions, customs and beliefs: Some traditional beliefs are often responsible for certain food habits and even child-rearing practices in the rural areas are responsible for this deficiency.
- Children with severe wasting may need to be admitted to the hospital for proper intervention, while those with stunting alone can be managed in the community.
- If the child is not able to take food by mouth, nasogastric tube feeding, intravenous infusion or parenteral nutrition is generally provided in hospitals.
- If signs indicate malabsorption, a gastroenterologist should be consulted. A pediatrician can also be consulted for pediatric cases.
- Vitamin supplementation may be provided even if there is no obvious sign of vitamin deficiency.
- If a stool examination reveals the presence of hookworm, roundworm or other intestinal parasites, then such cases should be treated with an appropriate anthelmintic drug.
- In susceptible areas of malaria, antimalarial treatment is also provided with chloroquine.
- Failure to grow at the expected rate, typically in terms of weight and height.
- Changes in behavior such as appearing unusually irritable or mental changes.
- Changes in physical attributes such as hair, skin colour, indigestion problems, oedema, wasting, hair changes etc.
- Child is having difficulty eating or drinking for many days.
Protein energy malnutrition (PEM) is a potentially fatal disorder of undernutrition in children. It is a leading cause of death in developing countries. It refers to a form of malnutrition where there is inadequate calorie or protein intake to meet the body’s demand. The deficiency might be primarily of protein when the diet provides adequate calorie but not sufficient to meet protein demand. It is called Kwashiorkor. It is often seen after a second baby is born and weaned off the breast milk but can appear any time during childhood. When both protein and energy are severely deficient, it is called Marasmus, which is less common than Kwashiorkor. It is a form of starvation. In developed countries PEM can develop in the homeless, psychiatric patients or patients with chronic debilitating illness like HIV/AIDS, cancer and GI disease, where nutrient absorption is impaired.
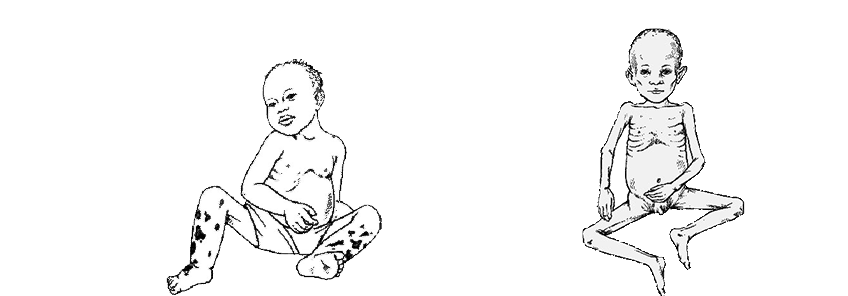
Kwashiorkor
Kwashiorkor is common between one and five years. Child who is weaned early and fed with food high in calorie but low in protein like (rice, yams, sweet potatoes only) are more likely to develop kwashiorkor. A child with this condition has significant fluid retention making them puffy and swollen. They have dry and peeling skin and have hair discoloration. Growth is retarded but less than that in marasmus.
Marasmus
Marasmus is characterized by gross wasting of muscle and subcutaneous tissues resulting in emaciation and marked stunting of growth but there is no fluid retention as in kwashiorkor. This condition develops in infants and very young children. The affected child’s body weight is less than 60 percentage of the expected for the age. Height is affected to the less extent while the fat in the adipose tissue is severely depleted.
If a child has both features of kwashiorkor and marasmus, then it is called Marasmic kwashiorkor.
Risk factors
Diagnosis
Severe PEM is usually obvious by clinical features and presence of risk factors. Your doctor will perform some physical examination such as, measuring height and weight and assessment of body fat stores like skin fold thickness. Further testing are usually not needed to make a diagnosis. Your doctor may also perform some tests to identify the cause of malnutrition depending on the specific circumstance.
Treatment
The patient of PEM must be evaluated for the severity of malnutrition, presence or absence of systemic infections and other nutritional deficiencies such as vitamin deficiencies, anemia, and fluid and electrolyte disturbances. The goal is to gradually increase the calorie and protein intake. These are some options:
When to visit the doctor
If you or your child is exhibiting the following signs, then you should immediately consult your with your doctor:



Send us your feedback on this article